Why is shopping for Medicare so complicated?
Editor’s Note: Journalist Philip Moeller, who writes widely on health and retirement, is here to provide the Medicare answers you need in “Ask Phil, the Medicare Maven.” Send your questions to Phil.
Unbelievably, the three recent Ask Phil columns about this year’s Medicare open enrollment season (Oct. 15 – Dec. 7) — un, deux, trois — did not answer all of your questions. In fact, some of you were brazen enough to disclose that you hadn’t even memorized these gems or — shocker — even read them!
After an extended session with an unsympathetic therapist, the Maven was able to limp back to his keyboard. There were two common themes in your missives — why is shopping for Medicare policies so complicated, and why must the drug companies charge such expensive prices?
Renee – Hawaii: On the Medicare.gov website I have been comparing drug plans. I have narrowed plans to those with identical drug tiers for the drugs I use and those with plan star ratings I thought acceptable. Deductibles are not a problem for me. For each plan, the preferred pharmacies and their convenience are acceptable. What else should I consider among the plans? Have I missed something? At this point is it logical for me to select a plan based on total cost as shown on the Medicare website?
MORE FROM MAKING SEN$E
Your guide to choosing a Medicare drug plan that’s right for you
Phil Moeller: Kudos to Renee for doing such a great job using Medicare’s Plan Finder website to figure out the best way to pick a Part D drug plan, either as a stand-alone choice or bundled in with a Medicare Advantage plan. The projected cost figures are only ballpark accurate, but still helpful. My only additional advice before selecting a plan is to visit the websites of your “finalists” and see how easy or hard it is to find information that you will need should you join that plan. Then I’d call the plan’s consumer hotline or contact number. Ask for details on how their plan works. What makes them better than other plans? Do they have any additional coverages not mentioned on Plan Finder? How helpful and knowledgeable is the person you speak to? If a plan doesn’t do a great job meeting your needs before you become a customer, imagine how disappointed you might be after you’ve purchased the policy.
Mary – N.Y.: I noticed in the back of the Medicare handbook that there are prices for all the Medicare Advantage plans with only one line devoted to where to go to find Medigap plans. This almost sounds like Medicare is pushing Medicare Advantage plans. Even on the Medicare website, it is hard to navigate to where you can compare Medigap plan prices and plan levels. Am I missing something?
Phil Moeller: Medicare does put out a very useful Medigap guide. And once you do find it, Medicare’s online shopping tool for Medigap is very helpful. But your point is well taken. Medicare Advantage plans do not work with Medigap, which is designed to supplement Original Medicare (Part A for hospital and Part B for doctor, outpatient and medical equipment). So any discussion of Medicare Advantage plans is not going to go into detail on Medigap. Further, Medigap policies are not regulated by Medicare, but by individual states, many of which have different rules and underwriting policies for Medigap. Always check your state’s insurance department website when researching Medigap options.
David – Nev.: I take one expensive drug and three low-cost generics. I have always had a Medicare supplement plan (Medigap), but I’m considering a Medicare Advantage plan to save money. What do you think?
Phil Moeller: Well, first off, I’m assuming you also must have a stand-alone Part D prescription drug plan, because Medigap doesn’t cover drugs. So I’m guessing your real question is whether an Medicare Advantage plan will cost you the same or less for the drugs you need, while its out-of-pocket annual maximum will give you catastrophic protection for less money than your Medigap plan. Based on your current health care needs, the answer is almost certainly yes — a Medicare Advantage plan with a bundled drug plan will be cheaper.
MORE FROM MAKING SEN$E
Which Medigap plan should you get?
But you shouldn’t stop there. What would happen if you needed a complex surgical procedure, faced an extended hospital stay or had to start taking one or more really expensive drugs? If you wanted to see the best specialty surgeon in the country for what ails you, for example, would this be covered under your Medicare Advantage plan? Probably not, but you should check before you get the plan. Ditto with having that procedure in a hospital 1,000 miles away that is renowned for the specialty care you need. As for really expensive drugs, both stand-alone Part D plans and bundled Medicare Advantage drug plans have the same catastrophic coverage, and you never have to pay more than 5 percent of the cost of drugs once you reach this stage of any Medicare drug plan.
Janice – Ill.: I’m totally tired of overpaying for my prescription drug coverage right now and for the last four years. I currently use only three cheap generics. I’m thinking of dropping Medicare Part D coverage entirely and going with a retail pharmacy discount plan with a $20 annual enrollment fee. Your thoughts, please.
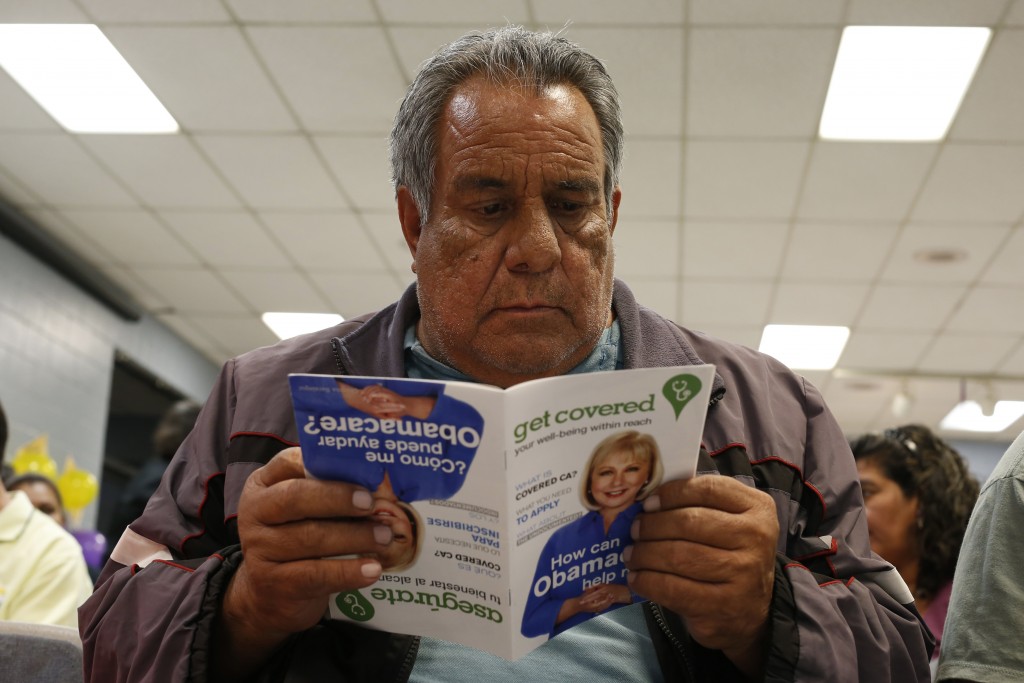
Phil Moeller: Healthy people with insurance wind up subsidizing sicker people with insurance. That’s the concept and reality of putting people into large risk pools, which is what Medicare (and the Affordable Care Act) do. Otherwise, only sick people would get insurance and their rates would be unaffordable. Having said that, I’m with you that drug prices are out of hand and that it’s time for Congress to give Medicare stronger tools to negotiate with pharmaceutical companies over prices.
For now, however, I would advise you not to end Part D coverage. If you do, you will face potentially stiff premium surcharges should you ever need Part D again. And as you get older, the odds grow that you will need this coverage. These surcharges will raise your Part D premiums by 1 percent for each month you’ve been without Part D coverage. These surcharges can be substantial if you’ve been without a plan for a long time, and the surcharges last for as long as you have a Part D plan. Instead of leaving Part D, use this year’s open enrollment period to find a plan with lower premiums. So long as your drug use remains modest, you will pay less, and by staying in Part D, you won’t later incur any of those nasty surcharges.
Julie – Wash.: I am 66, and my husband is 67. We are high earners and pay $405 for our Part B premiums every month and another $167 for a Medicare Advantage plan. We just learned that our plan is dropping our physicians’ group practice next year, and we are so bummed. Should we stay with the plan, keep seeing our doctors and pay a lot more for out-of-network charges, or should we switch to another plan? We are very light users of health care, are in good health and take only one prescription medication. I have to say, this whole thing amazes me. We own a business and provide health care to 26 employees. Their insurance is far more straightforward than this!
MORE FROM MAKING SEN$E
Everything you need to know about Medicare’s open enrollment
Phil Moeller: The only thing clear here is that Medicare’s excessive complexity is totally unacceptable. Whether it’s income taxes, Social Security or health care, years and years of government regulation inevitably lead to programs so complicated that we need to hire professionals to navigate them for us. Even if some or, arguably, a lot of this complexity results from efforts to be fair, the resulting bureaucratic behemoths are not in anyone’s best interest. As for your own situation, I’d first find out the Medicare plans your preferred doctors are still working with. How do their premiums and other policy provisions compare with your current plan? If there are no Medicare Advantage plans available to you, research the costs and other implications of using Original Medicare, a Medigap plan and a Part D drug plan. Millions of people do this. If you don’t like the costs and hassles of dealing with multiple Medicare plans and you want to keep seeing your doctors, paying out-of-network charges may be unavoidable.
R.S. – Tex.: At present, I am in good health, except for chronic reflux disease, and am not on any expensive daily medications. I am 68 years old and am covered by Medicare Part A and Part B. With the idea in mind that one could meet with a catastrophic illness at any time, my concern (I’m not losing sleep over this) is regarding the potential of the 20 percent that is not covered by Medicare if the need arises. Are Medicare Advantage plans intended to provide coverage of the not-covered 20 percent? My primary care doctor accepts Medicare and is part of a group practice that also accepts Medicare. He suggested that it would be prudent for me to check into a plan that covers the missing 20 percent.
Phil Moeller: As with Renee, the Maven would like to send a shout-out to R.S. for asking the right question. His doctor gets a gold star, too, for bringing up the issue of medical expenses. We call it Medicare health insurance, but it’s not. It’s sickness insurance. A smart way to shop for any insurance is to find out how you would fare in a worst-case situation. For Medicare, this means expensive and extended treatments that usually involve some kind of specialized surgery, hospitalization, skilled nursing care and expensive drugs. Medicare Advantage plans include annual caps on health expenses. So they certainly do provide protection against Original Medicare’s 20 percent coverage exposure, following copays for an initial amount of covered expenses. But that’s not the last word here. Many Medicare Advantage plans feature narrow networks of doctors and hospitals that can provide care. But such plans may expose you to potentially large out-of-network charges. The most common Medicare Advantage plans are health maintenance organizations (HMOs). There also are Medicare Advantage plans that include preferred provider organizations (PPOs). These PPO plans may provide you expanded access to specialists you might need were you to face a serious health issue. They also usually include an annual out-of-pocket maximum for non-network care. If you find an Medicare Advantage plan you like, you should call before signing up and find out exactly what kind of access and cost exposure you would have in the case of specialty doctors and hospitals, should you need them.
Thomas – Mich.: I am currently 65 years old and have health benefits through my wife’s employer. In February 2016, I will turn 66 and will continue to work, and so will my wife. Can I then collect full Social Security benefits at 66 while being highly compensated? Do I have to sign up for Medicare A and B to collect Social Security?
Phil Moeller: Social Security’s earnings test ends when you reach full retirement age, which is age 66 right now. So regardless of how large your wage income is, your Social Security benefits will not be even temporarily reduced should you begin taking them at 66. However, as you may know, your Social Security benefits will rise by 32 percent between the ages of 66 and 70 if you can afford to delay them until then. Lastly, you do not have to sign up for Medicare to begin receiving Social Security, but you will be automatically enrolled in Medicare Part A when you begin receiving Social Security payments. Technically, this means you will be on Medicare, although you need not sign up for Part B or other parts of Medicare so long as you continue to be covered on your wife’s employer group health plan (assuming her employer has more than 20 employees).
ncG1vNJzZmivp6x7sa7SZ6arn1%2Bjsri%2Fx6isq2eVmLyvu8yyZqqtlajBqrvNrGSmnZSesKK%2BxGamqZ2eYrKvvs6lo6adnqk%3D